Exciting new advancements in the care of cancer patients are changing the way the disease is treated. Surgery, radiation and chemotherapy have long served as the three pillars of cancer treatment, but recent years have ushered in a fourth (targeted therapies) as well as a fifth (immunotherapy) which harnesses the patient’s own immune system to fight the disease. CAR-T cell therapy, which is a type of immunotherapy, is a relatively new treatment that was approved by the FDA in 2017 to treat adult patients with advanced lymphomas and children with acute lymphoblastic leukemia who have failed to respond to two previous lines of treatment. This therapy has successfully achieved remission for patients who were previously considered terminal.
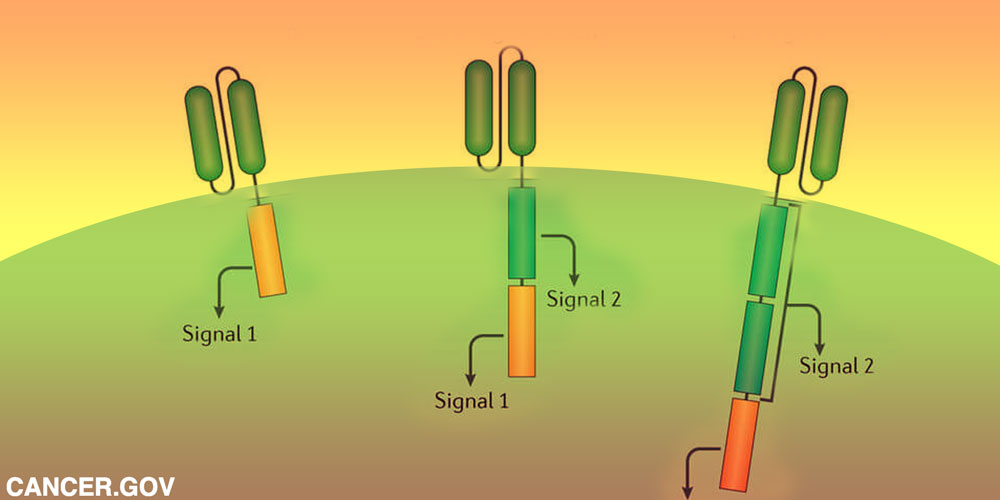
This particular immunotherapeutic treatment is a type of adoptive cell transfer therapy called CAR-T cell therapy or chimeric antigen receptor t-cell therapy. With this treatment the patient’s blood is drawn and a type of immune cells called T-cells (white blood cells that are crucial to orchestrating attacks on infected cells) are separated from the sample. In the lab these cells are reprogrammed with a disarmed virus that causes them to produce a synthetic molecule called a CAR (chimeric antigen receptor). The modified cells are then “expanded” in the lab by hundreds of millions and then re-infused into the patient. Once returned to the bloodstream, they continue to multiply, newly armed with the ability to recognize a specific protein (antigen) called CD19 that resides on the surface of the tumor cells.
Even though there has been great success in targeting CD19, cancer’s ability to mutate (and even shed CD19) in order avoid detection, necessitates that the technology expand to target other molecules. Doing so will increase avenues of attack, thus potentiating better patient outcomes. Other molecules are being researched and there is some success, but none has been as effectively attacked as CD19. As with most treatments, there are some troubling side effects and CAR-T cell treatment is no different. One of the most common complications is cytokine release syndrome, which happens when T-cells rapidly release a massive amount of cytokines (chemicals) into the bloodstream. This can cause dangerously high fevers and drops in blood pressure. Fortunately, this condition can usually be managed. Other concerns are massive die-offs of anti-body producing B-cells (which are treated with immunoglobulin), cerebral edema (swelling), confusion and seizure-like activity. All of these conditions can usually be reversed.
Currently, CAR-T cell treatment is only available for a few conditions that haven’t responded to previous therapies. Because it has been effective at achieving remission in patients who were once considered terminal, it is bound to become more widely available. Researchers are even investigating the possibility of creating products from the blood supply of healthy people that can be used as needed. Until these advances come to pass, people who are interested in receiving CAR-T cell therapy can find more information about its applications at clinicaltrials.gov.
Some of the links on this website are affiliate links, and as an Amazon Associate, we may earn an affiliate commission from qualifying purchases – at no cost to you.
This website is for informational and/or entertainment purposes only and is not a substitute for medical advice, diagnosis, or treatment.
© 2025 Drew Pinsky Inc. | All Rights Reserved
Get alerts from Dr. Drew about important guests, upcoming events, and when to call in to the show.
For text alerts, msg and data rates may apply